Patient Health Questionnaire 9 (PHQ-9)
Recommended frequency: Every 2 weeks
Summary
The Patient Health Questionnaire 9 (“PHQ-9”) is a multi-purpose measure used to identify and monitor depression severity. It is a brief, 9-item version of the original PHQ assessment, which measures a variety of mental health challenges in addition to depression, such as anxiety, panic disorder, sleep disorders, and more. The PHQ-9 was co-created by Drs. Robert L. Spitzer, Janet W.B. Williams and Kurt Kroenke in 1999.
About the PHQ-9
The PHQ-9 combines depression diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) with other leading major depressive symptoms. The key diagnostic symptom criteria adapted from the DSM-IV includes:
- Two typical signs of depression: anhedonia (referring to the inability or reduced ability to experience pleasure) and depressed mood;
- Cognitions (e.g. guilt/worthlessness and suicidality/thoughts of death); and
- Physical symptoms (e.g. change in appetite, difficulty sleeping and concentrating, feeling tired/slowed down or restless).
Each of the 9 questions rate the frequency of the symptoms, which factors into the severity index.
Clinicians and clinical leaders will often ask about the differences between the PHQ-9 and other depression scales. In comparison to the other commonly used depression scales (BDI, HAD-D, QIDS), the confidence intervals are quite similar, meaning they have all demonstrated reliability, validity, and are responsive to change. The PHQ-9 has a particularly high validity score, such that when PHQ-9 scores were above 10, the measure was shown to have a sensitivity of 88% and a specificity of 88% for Major Depressive Disorder—meaning that a score above 10 was a good indication that a diagnosis of depression would occur. Each of the major depression scales have their differences, although the PHQ-9 and BDI-II in particular tend to measure relatively equal levels of severity and track symptom change in a similar manner. The PHQ-9 is often preferred to other comparable assessments due to its brevity, which makes it easy to integrate into research or practice, and helps promote high completion rates.
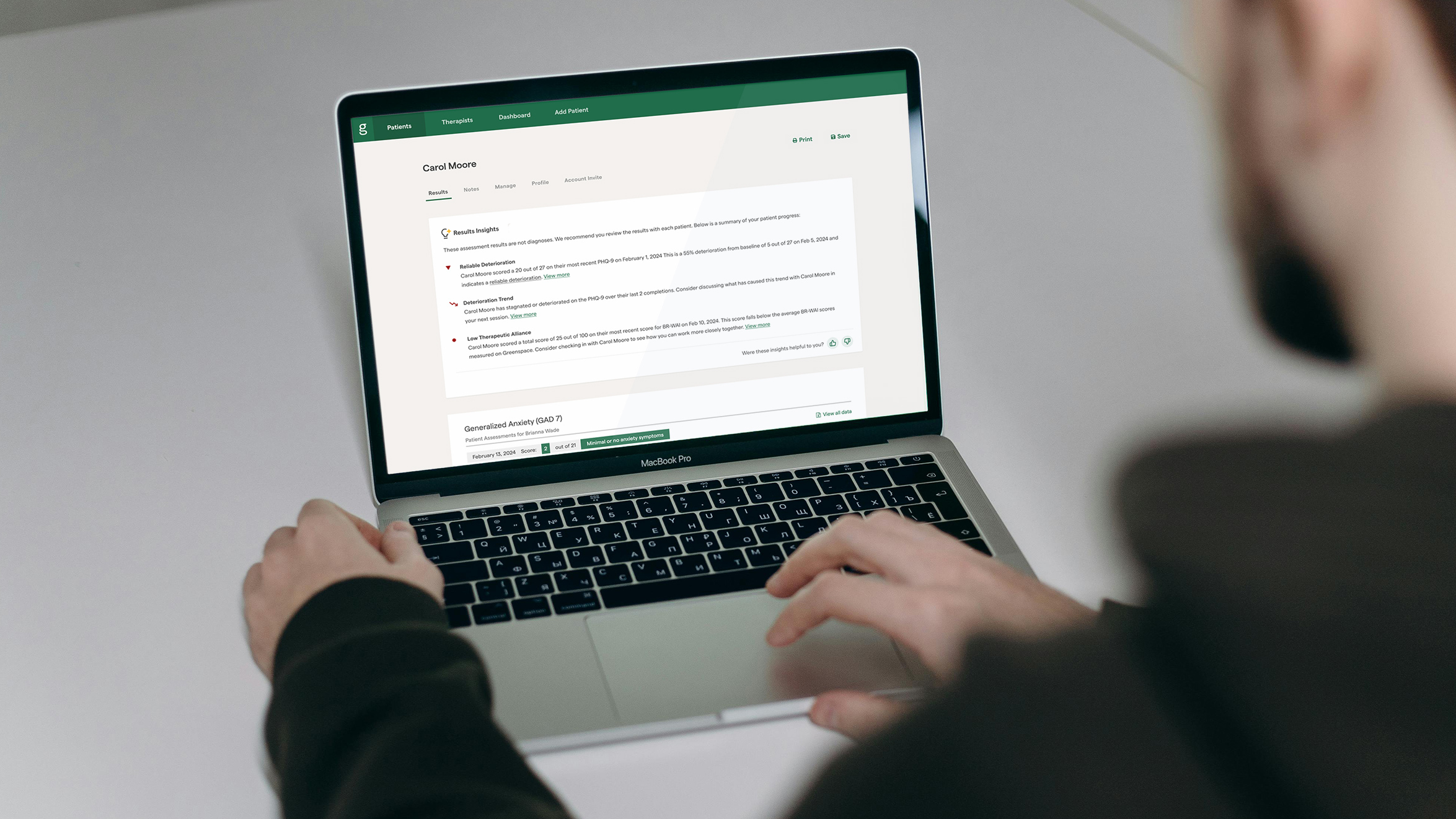
Assessment Insights
Check out more than 40 Assessment Guides with information and insights on the most popular assessments used on the Greenspace MBC Platform. Explore the categories below to find assessments you may be interested in learning more about.
Back to the hub