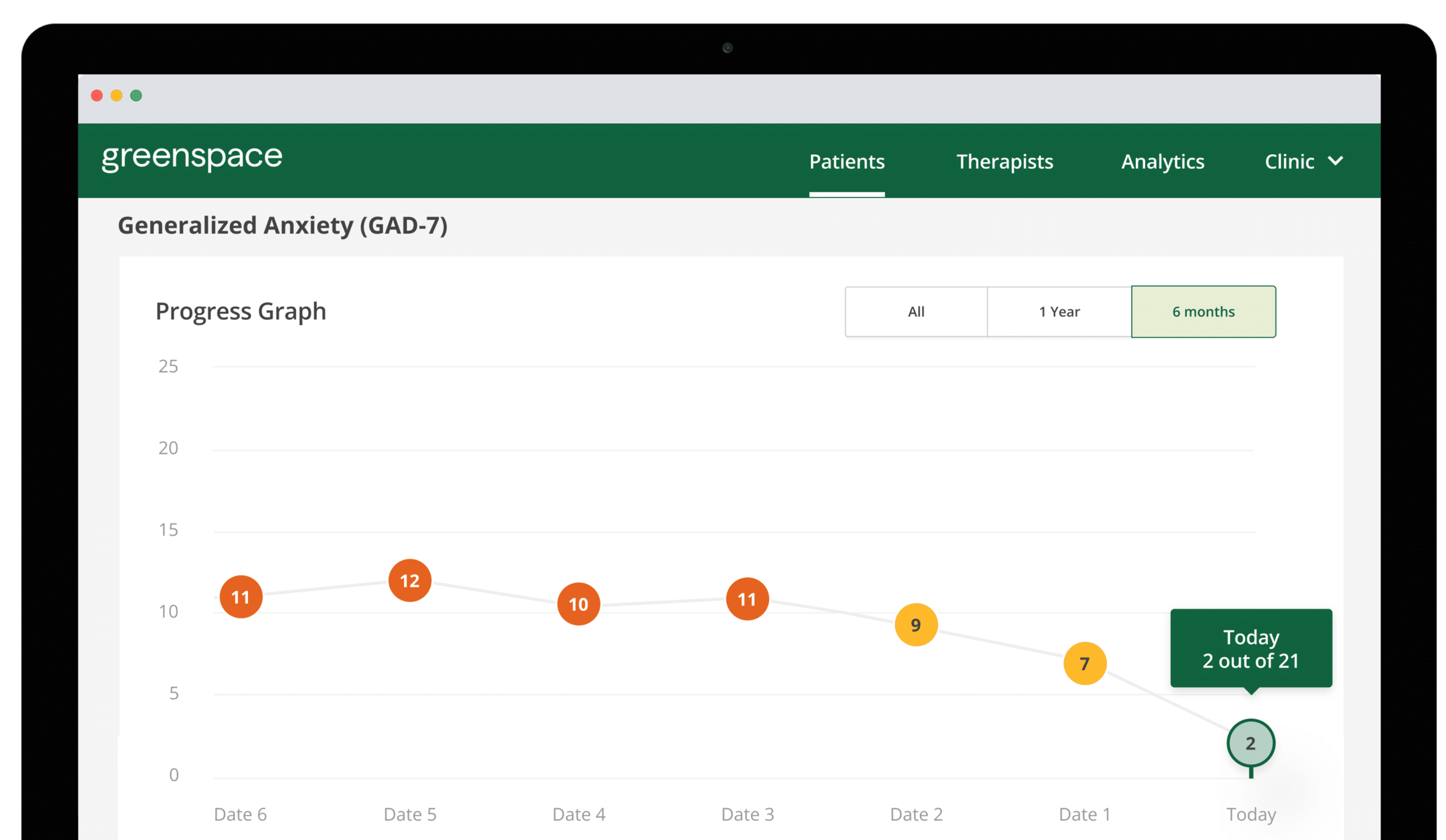
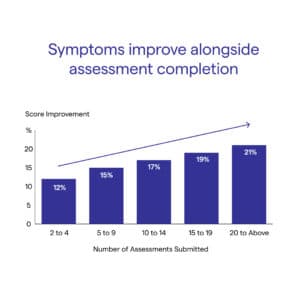
Boost member satisfaction and improve outcomes across your membership through data-driven, personalized care at scale. Whether it’s Medicare, Medicaid, or commercial populations, our population health hub enables early identification of need, timely support, and clear pathways to care, while maintaining an auditable record of screening, follow-up, and confirmation of care. For Medicare plans, this same foundation directly supports enhanced Star Ratings. Real-time analytics and population-level visibility allow plans to surface gaps in care delivery and leverage usage and outcome data to inform continuous quality improvement. By better supporting members throughout their care journey, plans improve outcomes, strengthen the member experience, and ensure their entire population receives timely, appropriate support.
Learn more